Bacteria have been in contact with antibiotics long before humans discovered them and began to use them to their benefit, since it is the microorganisms themselves that naturally produce these compounds to protect themselves from other microbes.1,2 Therefore, they have developed different mechanisms to protect themselves from the effect of antibiotics and render them ineffective. The main mechanisms of resistance by which an antibiotic ceases to be effective are:3
- Modification of the antibiotic molecule. Bacteria are capable of producing enzymes that produce chemical alterations or even destruction of the molecule, as in the case of β-lactamases.
- Membrane impermeability. Many antibiotics have their target in the cytoplasm of bacteria, if the membrane becomes more impermeable and the antibiotic is not able to penetrate inside the cell it will not be able to exert its effect.
- Production of efflux pumps. In some cases, bacteria are able to produce efflux pumps that expel the antibiotic out of the cell, preventing its interaction with the target.
- Target modification. By modifying the structure of the antibiotic target, bacteria prevent its interaction and, therefore, the effect of the antibiotic.
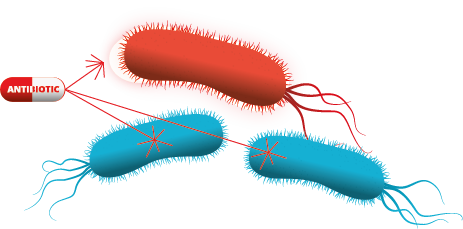
Mechanisms of antibiotics resistance
Mechanisms of resistance acquisition: How is antibiotic resistance generated and transmitted?
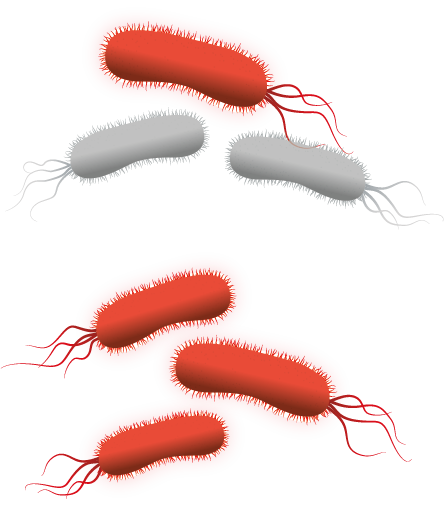
These antibiotic defense mechanisms can be generated spontaneously, by mutations in the DNA of bacteria, but they can also be transmitted from one bacteria to another.
Bacteria create exact copies of themselves when they divide, therefore, if in a bacterial population sensitive to an antibiotic a bacterium mutates and generates resistance, it will be able to generate a new bacterial population in which all the bacteria have this resistance. This is the main reason why it is so important to use antibiotics correctly, respecting the recommended administration and exposure times. An incubation period with the antibiotic shorter than necessary will result in the inhibition of the most sensitive bacteria, while the most resistant bacteria will continue to multiply, generating a new population of resistant bacteria. On the other hand, overexposure to antibiotics for a prolonged period of time, promoted in recent years by humans, is increasing the appearance of resistance by forcing bacteria to adapt to the environment in order to survive.
The second pathway by which bacteria can acquire resistance is by horizontal gene transfer. This gene transfer can occur in four ways:3,4
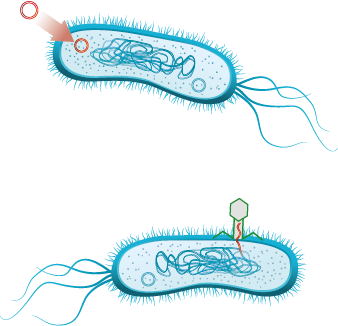
- Transformation. It occurs when a bacterium incorporates genetic material from its environment, usually circular DNA molecules (plasmids) that have been released by other bacteria.
- Transduction. This form of genetic exchange is mediated by bacteriophage viruses, those capable of infecting bacteria. When a bacteriophage virus infects a bacterium, it can accidentally carry with it part of the genetic material of that bacterium and, by infecting a new bacterial cell, pass this piece of DNA to it. Therefore, if the piece of DNA contains an antibiotic resistance gene, the new bacterium will also become resistant.
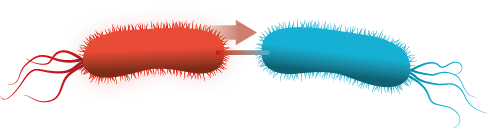
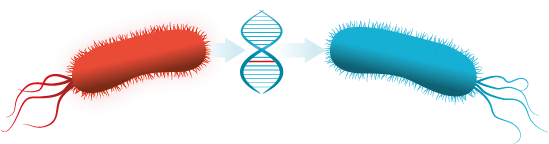
- Conjugation. Conjugation occurs when genetic material is exchanged between two bacteria through a channel called the pilus. Through this conduit, the donor bacterium transfers genetic material, usually in the form of a plasmid, to the recipient bacterium.
- Transposon or jumping gene. These are transposable genetic elements, i.e., they can move from one place to another within the genome. In a bacterium, if one of these transposable elements “jumps” from the chromosome to a plasmid, the genes it carries can easily be transmitted to other bacteria by transformation or conjugation. These elements sometimes carry pathogenicity and antibiotic resistance genes that can spread rapidly through the population.
References
- Patil, S.M., and Patel, P. (2021). Bactericidal and Bacteriostatic Antibiotics (Infections and Sepsis Development).
- Waksman, S.A. (1947). What is an antibiotic or an antibiotic substance? Mycologia 39, 565–569.
- Munita, J.M., and Arias, C.A. (2016). Mechanisms of Antibiotic Resistance. Microbiol Spectr 4. https://doi.org/10.1128/microbiolspec.VMBF-0016-2015.
- Arnold, B.J., Huang, I.-T., and Hanage, W.P. (2022). Horizontal gene transfer and adaptive evolution in bacteria. Nat Rev Microbiol 20, 206–218.




