The discovery, commercialization and administration of antimicrobial compounds to treat infections in humans, animals and plants has revolutionized modern medicine. These antimicrobials include antibiotics, antivirals, antifungals and antiparasitics, which are used to treat infections caused by bacteria, viruses, fungi and parasites, respectively.1
Antimicrobial resistance occurs when these microorganisms no longer respond to the drugs. As a result, antimicrobials become ineffective, and infections become difficult or even impossible to treat, increasing the risk of disease spread and even causing death.2
Antibiotics, the group of antimicrobial compounds intended to prevent and treat infections caused by bacteria, has become one of the most widely used medicines in the field of health, but their indiscriminate use is increasing the generation of resistance. Although antibiotic resistance is a natural process that occurs over time through genetic changes in bacteria, human activity is accelerating its appearance and spread, putting health at risk, reducing farm productivity and threatening food safety.2
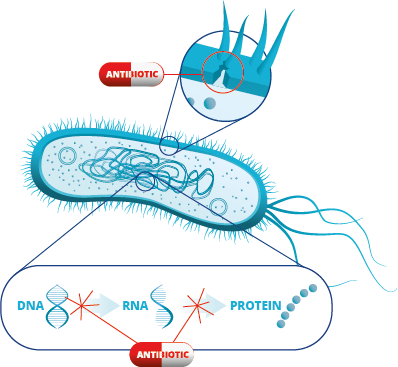
To understand the importance of the problem of antibiotic resistance, it is first necessary to understand how antibiotics affect bacteria, and what mechanisms bacteria use to inactivate them.
Mechanisms of action of antibiotics: How do antibiotics affect bacterial cells?
The first thing is to differentiate between bacteriostatic and bactericidal antibiotics. A bacteriostatic compound is one that inhibits bacterial growth, while a bactericidal3,4 compound is one that kills bacterial cells. Understanding this concept is key to understanding the mechanism of action of antibiotics, which will help us to choose the most appropriate antibiotics and effective concentrations.
The mechanisms of action of antibiotics are based on the inhibition or alteration of the different cellular components necessary for cell survival. The four main ways in which antibiotics affect bacterial cells are: alteration or inhibition of bacterial wall synthesis, inhibition of RNA transcription, inhibition of protein synthesis and inhibition of DNA replication.5
References
- Munita, J.M., and Arias, C.A. (2016). Mechanisms of Antibiotic Resistance. Microbiol Spectr 4. https://doi.org/10.1128/microbiolspec.VMBF-0016-2015.
- Pabst, S. (2023). Antimicrobial resistance. Worl Health Organization. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance.
- Patil, S.M., and Patel, P. (2021). Bactericidal and Bacteriostatic Antibiotics (Infections and Sepsis Development).
- Nemeth, J., Oesch, G., and Kuster, S.P. (2015). Bacteriostatic versus bactericidal antibiotics for patients with serious bacterial infections: systematic review and meta-analysis. Journal of Antimicrobial Chemotherapy 70, 382–395.
- How Bacteria Build Resistance at the Cellular Level (2017). Milken Institute School of Public Health. https://onlinepublichealth.gwu.edu/resources/antibiotic-resistance-at-cellular-level/.




